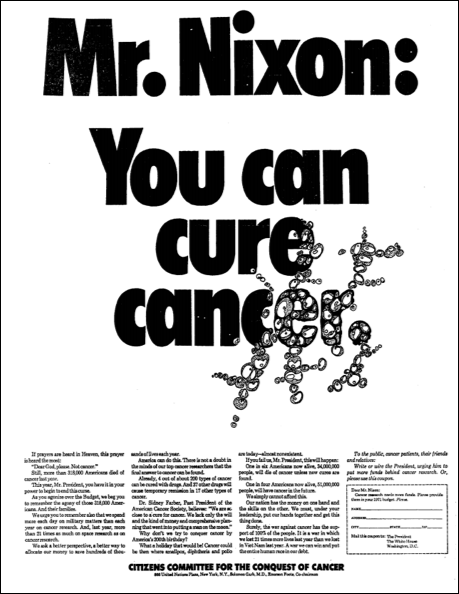
Cancer Advocates Published An Ad In 1969 Calling For Curing Cancer To Become A National Priority, Which Lead To Increased Federal Funding For Research.
Those still left behind in the war on cancer are top of mind as we recognize Blood Cancer Awareness Month. The entire month of September provides advocates such as Louis DeGennaro, Ph.D., President and CEO of The Leukemia & Lymphoma Society (LLS), an opportunity to highlight the unmet needs of the estimated 1.4 million people in the U.S. who are either living with or are in remission from blood cancer.
“I’m glad we can acknowledge we have had great success in many blood cancers,” DeGennaro said. “We truly have made remarkable progress. But some of the remaining challenges we face are due to the vast complexity of the diseases.”
Those complexities are now forcing advocates like him into new roles in developing new treatment options for patients.
More Complex Than We Thought
While the advocates who petitioned President Nixon 50 years ago suggested that cancer could be conquered within a matter of years, the disease proved to be a far more formidable foe.
Blood cancer is a complex family of many diseases—including leukemia, lymphoma, multiple myeloma, myelodysplastic syndromes (MDS) and myeloproliferative neoplasms (MPNs)—each with its own subtypes.