“Myelofibrosis is a serious and often debilitating disease for which there has only been one approved treatment option for nearly a decade,” said Dr. Claire Harrison, a hematologist at an NHS Foundation Trust in London.
“It took us a long time to realize a mutation in JAK2 was responsible for the majority of patients with myelofibrosis, but once it was discovered, it opened a whole new area of exploration in the field.”
Harrison and others are still uncovering the mysteries behind JAK2, but what they already know is changing how doctors treat patients with myelofibrosis.
First impressions of the JAK2 gene mutation
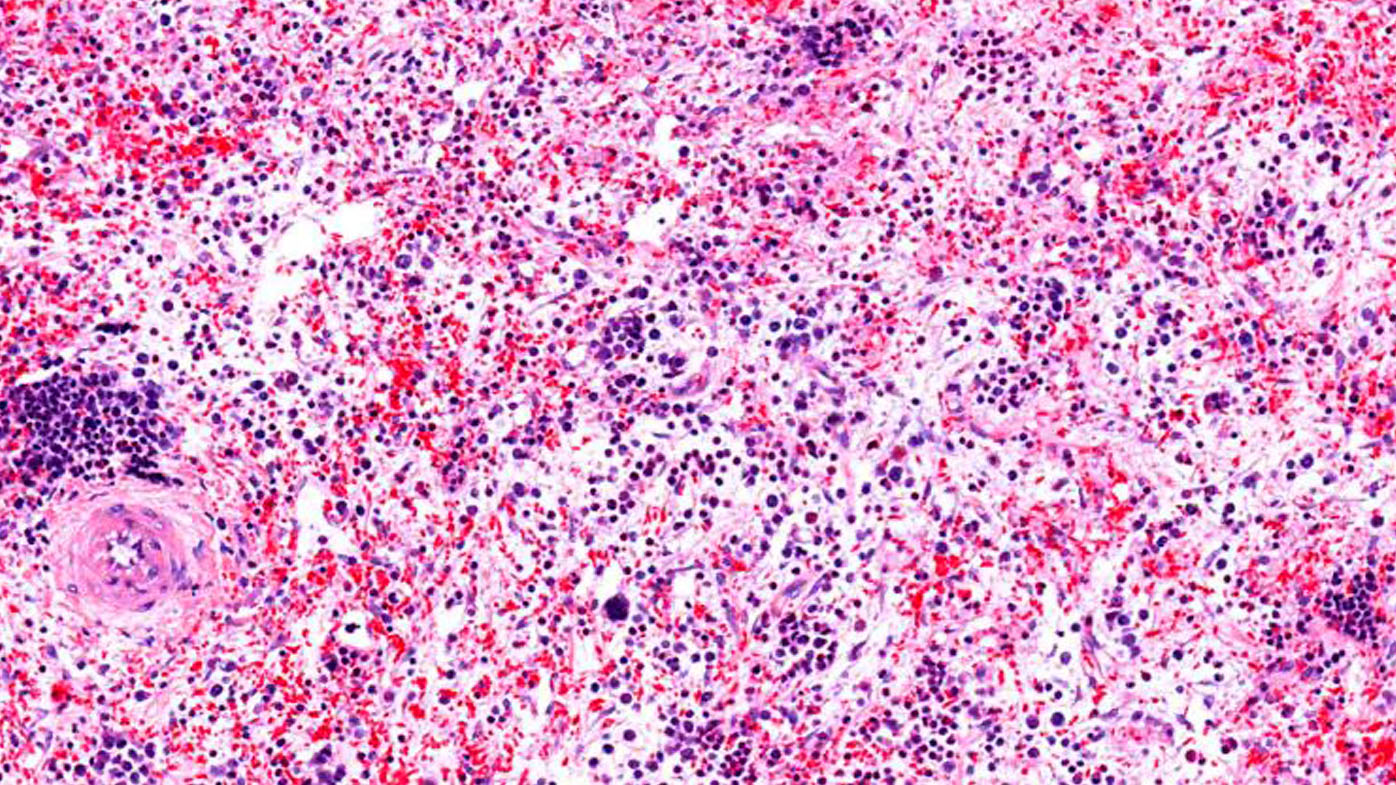
JAK2 was first identified 30 years ago in a shotgun approach to identify anything resembling a family of enzymes known at the time for prompting cell growth and development. The researchers found JAK2 in a line of perpetually youthful cells that give rise to blood cells. “JAK2 is important for the production of healthy blood cells,” explained Harrison. In a mouse model, for example, if you remove the JAK2 gene, the mouse cannot produce enough blood cells and will not survive.”
Since then, plenty more has been learned about its role in developing blood cells. In 2005, researchers discovered that about half of patients with myelofibrosis had a specific mutation of JAK2—V617F. Furthermore, they discovered that those with the V617F mutation did not live as long after diagnosis as those without that particular genetic mutation.
“The V617F mutation is by far the most common mutation seen in myelofibrosis,” said Harrison. “JAK2 molecular testing has become standard in the work up and diagnosis of myelofibrosis and other myeloproliferative diseases.”


