The critical role of patient samples in cancer research
Patient samples are any type of biopsy or specimen (e.g., tissue, blood, etc.) collected from a patient by their healthcare team. Samples are routinely collected during patient care and treatment and can then be studied by their treatment team and other researchers. Patient samples can provide a wealth of information for cancer research, guiding aspects from early target identification to biomarker analysis for patient stratification. The data patient samples provide are unique and cannot be duplicated by other methods of research.
The tumor microenvironment (TME), which is the complex network of cells and tissues that surround a tumor, is integral to cancer cell survival and growth. This environment is specific to the cancer residing inside the human body. As such, studying cancer cells in vitro – cell lines that can be studied outside of the body in a laboratory setting – or in other models may, in some instances, fall short when results are extrapolated to human tumors.
“The translation between what's going on in a test tube or Petri dish to what's going on in a human patient is really not a direct comparison,” said Scott Ely, scientific director, Translational Pathology. “There are many examples of a drug having been developed that is effective in vitro or in other models but that doesn't work in humans.”
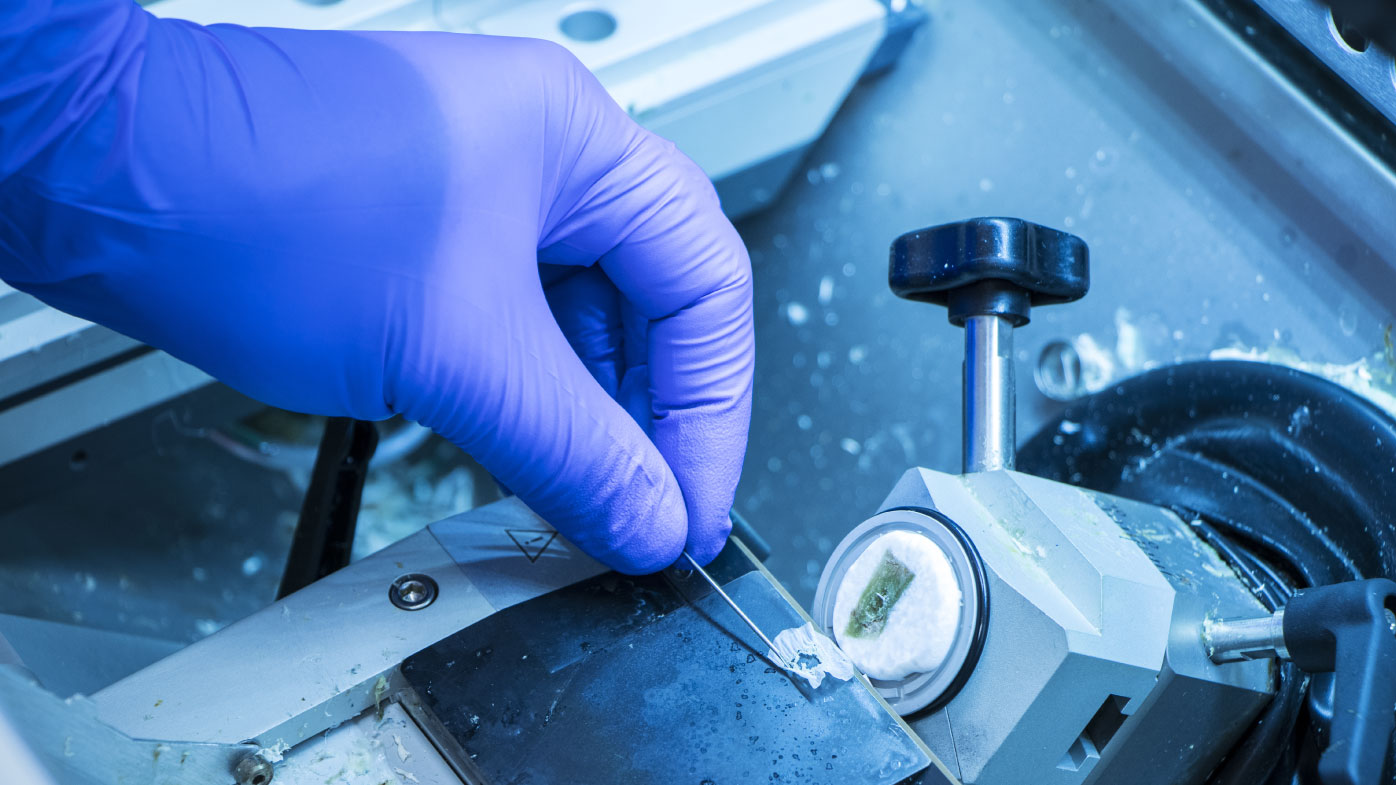
In many instances, an effective way to understand what is happening in a particular patient’s cancer, at a specific point in time, is to take a sample from the patient’s body — blood, tissue, etc. — anywhere the cancer cells may exist. This biopsy provides the opportunity to interrogate the properties of the tumor as well as the interactions of various cell types and the landscape within which the tumor exists. Specific anti-cancer targets can be identified and examined, helping researchers to study and understand the role a target plays in the TME and how it may contribute to cancer cell growth.
Scientists can take these samples and study them for biological markers — biomarkers of the particular type of cancer. Data from these biomarkers can also be used to pinpoint specific patient populations in whom a therapeutic could be effective, or ineffective, to better match patients to specific therapies.
“We use biopsy samples to understand whether a specific protein is expressed in the tumor cells or other cells in the microenvironment,” said Scott Ely, scientific director, Translational Pathology, Translational Medicine. “Understanding the expression of certain targets tells us whether a patient is a good candidate to respond to a certain therapy or not and can help get them into the right trial. Moreover, understanding the expression of a target, not only in the tumor, but in immune cells and normal cells, will give us a better understanding of expected off-target effects. It also helps us understand the mechanism of action of a drug. With good biopsies, we actually know what is going on inside a patient.”
To stay ahead in the cancer fight, it is also critical to profile patient samples over time throughout treatment to discover mechanisms of cancer resistance that can be further mitigated. For this purpose, Ely emphasizes the utility of blood-based liquid biopsy collection.
These learnings apply at all stages of preclinical and clinical development and are key to the application of translational medicine, which integrates scientific understanding into decision-making with the goal of accelerating the discovery and development of new medicines for patients.
The unique challenges of working with patient samples
Patient samples can provide a wealth of information for drug development, but working with these delicate specimens can present challenges. The most pressing challenges to the industry involve controlling pre-analytic variables and obtaining a workable sample size.